Afterload Stress and Preload Reserve
- Left ventricular size or preload is a determinant of the SV and afterload.
- Normally, the LV compensates for increases in afterload by increases in preload.
- The increase in end-diastolic fiber stretch or radius further increases wall tension in accordance with Laplace’s law, resulting in a reciprocal decline in myocardial fiber shortening (ie, inverse force-velocity relationship).
- Despite the relative decline in fiber shortening, the SV is maintained because contractile force is augmented at the higher preload (ie, Starling or length-active tension effect).
- The increased contractility at higher LVEDVs may be mediated by an increased sensitivity to the inotropic effects of extracellular calcium at longer muscle lengths.
- Use of this preload reserve allows the LV to maintain its SV in the face of an afterload stress.

The increase in afterload (ie, beat 2) elicits a compensatory increase in end-diastolic volume (EDV) (ie, beat 3), preserving SV at the higher afterload. However, when the ventricle reaches the limit of its preload reserve, it overdistends, and preload behaves as if it were fixed. SV then decreases with further increases in the systolic pressure (ie, afterload mismatch; beat 4), a clinical corollary of the inverse force-velocity relation.
Ref: KAPLAN’S CARDIAC ANESTHESIA 7 TH EDITION
Pressure-Volume Loops

The pressure and volume changes that occur during a normal cardiac cycle are depicted
A pressure-volume loop is generated when ventricular volumes are plotted against simultaneously occurring ventricular pressures for a single contraction
Phase 1 shows ventricular filling and represents loading of the heart before contraction (ie, preload). During early and middle diastole, filling of the ventricle is rapid, depending on the pressure gradient between the left atrium and the LV. In late diastole, the left atrium contracts (ie, a wave), which results in the final left ventricular enddiastolic
volume (LVEDV) and pressure (LVEDP). Atrial contraction in the normal heart accounts for 15% to 20% of ventricular filling. The normal ventricle accommodates large changes in ventricular volume with only a small change in ventricular diastolic pressure.
Phase 2 Ventricular systole occurs in the isovolumic and ejection phases. During isovolumic (isometric) systole, intraventricular pressure increases dramatically. However, there is little or no concurrent decrease in ventricular volume because the aortic valve is still closed.
Phase 3 is the systolic ejection period. When intraventricular pressure exceeds aortic pressure, the aortic valve opens, and ejection begins. At the end of phase 3, the aortic valve closes. This point is the end-systolic pressure-volume coordinate, which may uniquely reflect the cardiac inotropic state.
Phase 4 Isovolumetric relaxation.

Ref: KAPLAN’S CARDIAC ANESTHESIA 7 th EDITION
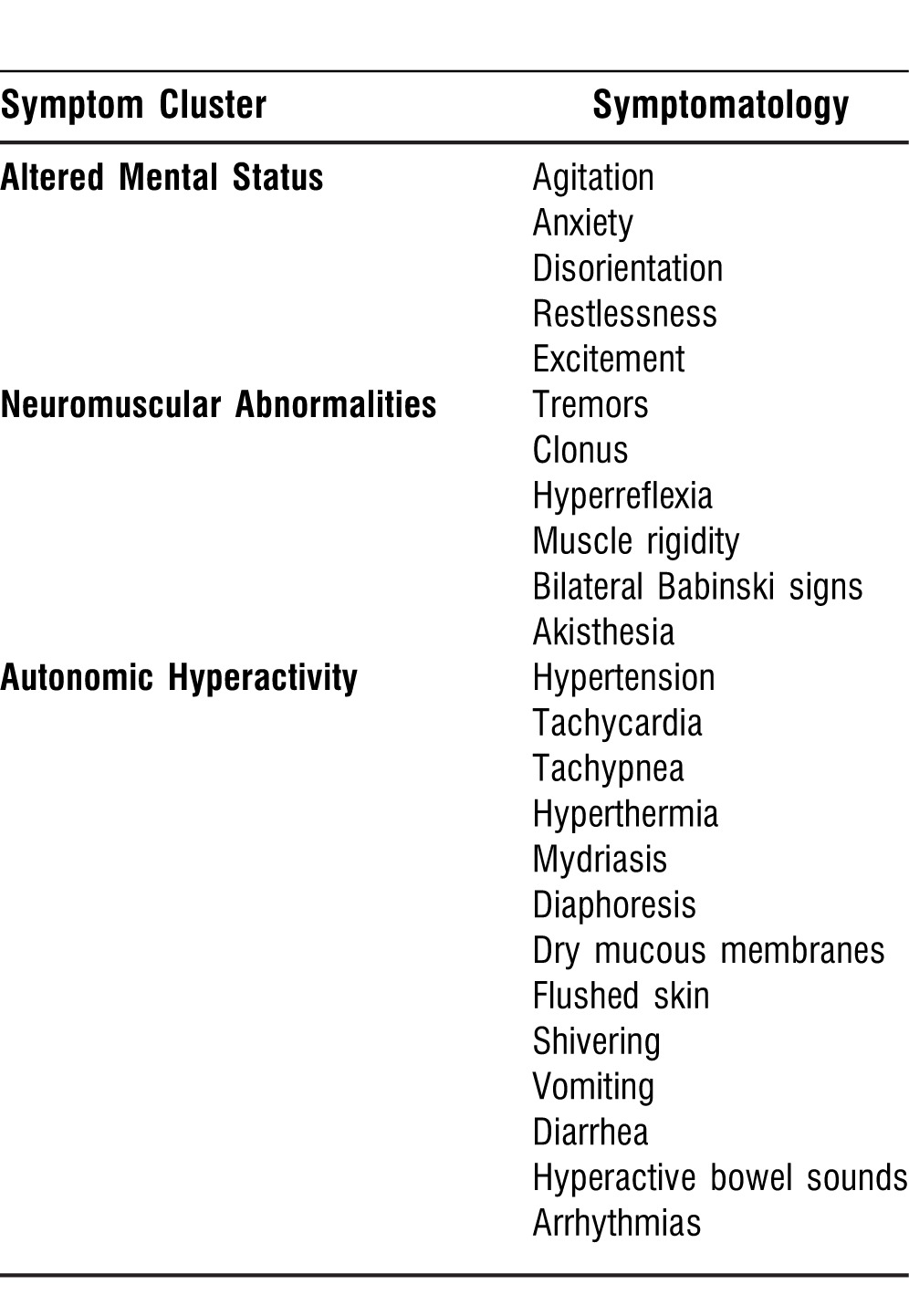
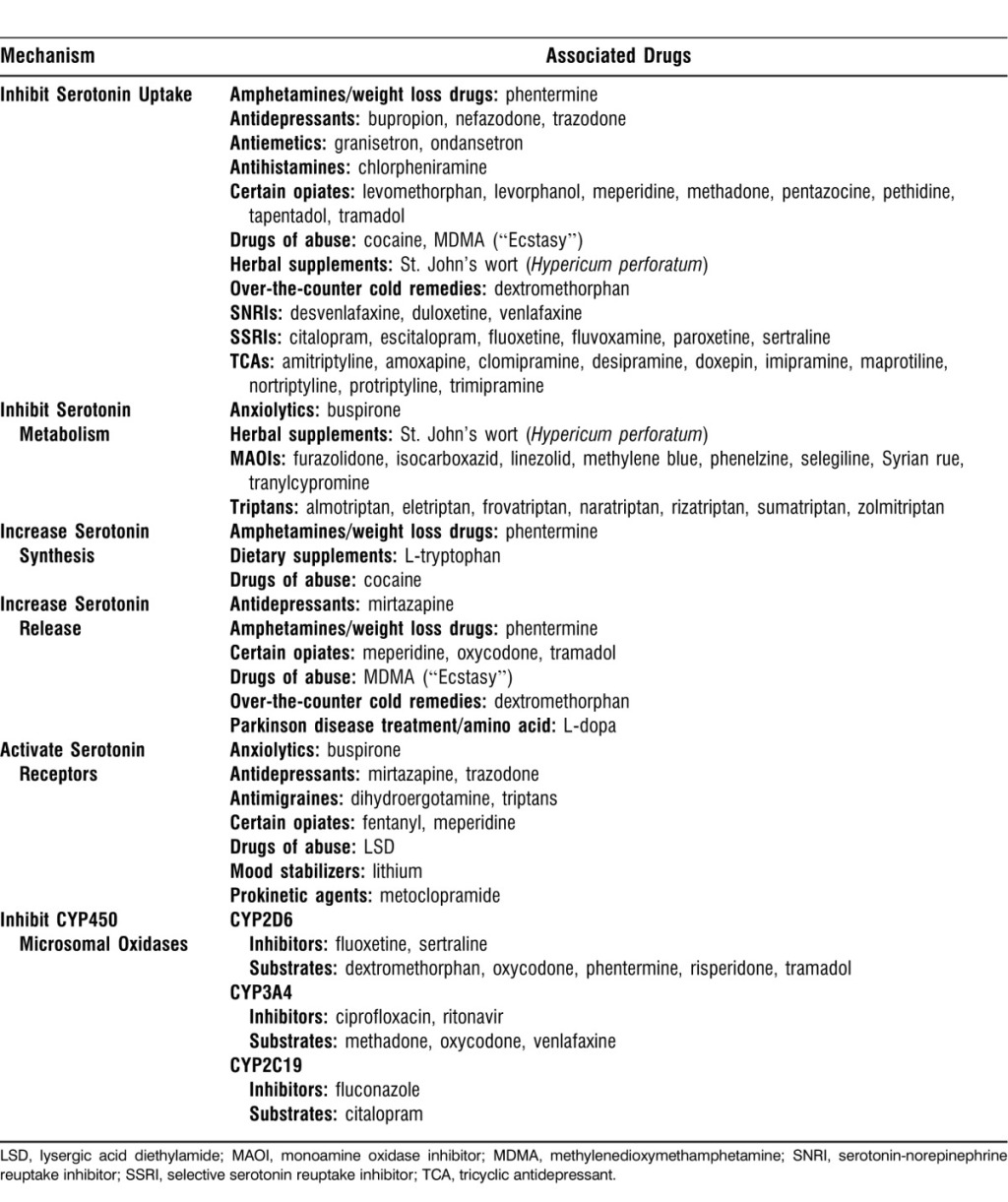
Serotonin Syndrome
Serotonin syndrome is a potentially life-threatening syndrome that is precipitated by the use of serotonergic drugs and overactivation of both the peripheral and central postsynaptic 5HT-1A and, most notably, 5HT-2A receptors. This syndrome consists of a combination of mental status changes, neuromuscular hyperactivity, and autonomic hyperactivity. Serotonin syndrome can occur via the therapeutic use of serotonergic drugs alone, an intentional overdose of serotonergic drugs, or classically, as a result of a complex drug interaction between two serotonergic drugs that work by different mechanisms. A multitude of drug combinations can result in serotonin syndrome.
Symptomatology Triad Associated With Serotonin Syndrome:
Differentiating Serotonin Syndrome Among Common Presentations:

Mechanisms of Serotonin Syndrome and the Drugs Associated with Each:
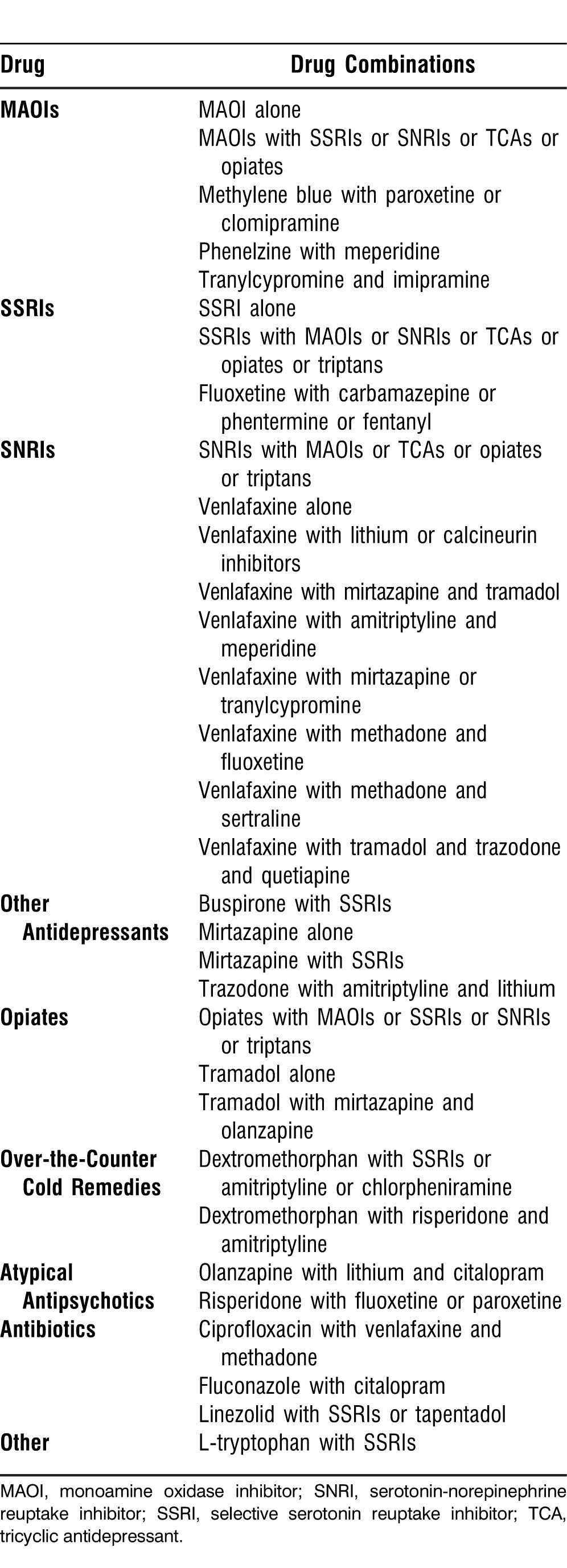
Reported Drug Combinations Causing Serotonin Syndrome:
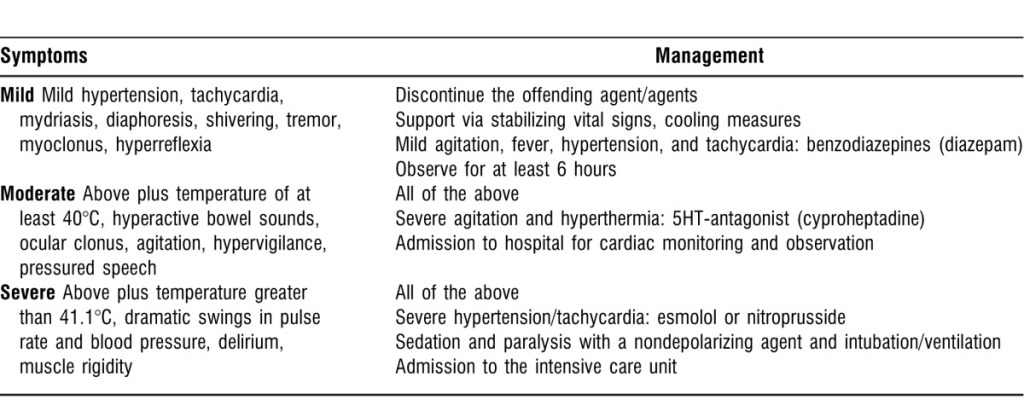
Management of Serotonin Syndrome:
Ref:

The management of hypotension with vasopressors during caesarean section under spinal anaesthesia
1. Hypotension following spinal or combined spinal-epidural anaesthesia at caesarean section causes both maternal and fetal/neonatal adverse effects. 2. Hypotension is frequent and, therefore, vasopressors should be used routinely and … Continue reading The management of hypotension with vasopressors during caesarean section under spinal anaesthesia
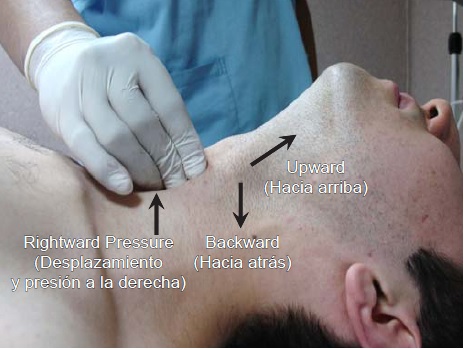
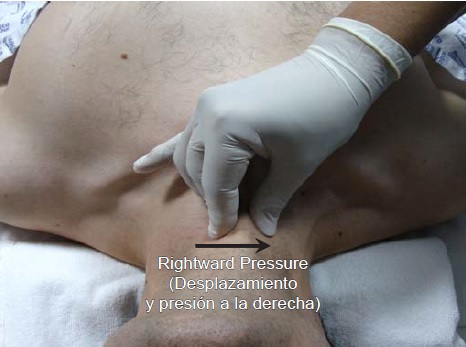
Retroclavicular approach of brachial plexus block
The Retroclavicular Approach to The Infraclavicular Region (RAPTIR) is a newly described USG brachial plexus block technique that optimizes sonographic needle visualization as a means of making regional anesthesia of the upper extremity safer and easier to perform. With RAPTIR a single well-visualized injection distant from key anatomic neck and thorax structures provides extensive upper extremity anesthesia, likely reducing the risk of complications such as diaphragm paralysis, central block, nerve injury, vascular puncture, and pneumothorax. Additionally, patient positioning for RAPTIR is well suited for the awake, acutely injured ED patient as the upper extremity remains adducted in a position of comfort at the patient’s side. Thus, RAPTIR is a potentially ideal combination of infraclavicular targeting, excellent needle visualization, single injection, safety, comprehensive upper extremity analgesia, rapid performance, and comfortable patient positioning.