Pain assessment tools The tools used are the: Numerical rating scale for children 5 years and above The Faces Pain Scale Revised for children aged 3 years and above The … Continue reading Paediatric Anaesthesia Formulas – 2


Pain assessment tools The tools used are the: Numerical rating scale for children 5 years and above The Faces Pain Scale Revised for children aged 3 years and above The … Continue reading Paediatric Anaesthesia Formulas – 2

Fluid requirements Fasting Guidelines for Pediatric Patients TYPE Fasting Time (hr) Clear liquids* 2 Breast milk 4 Infant formula 6† Solid (fatty or fried) foods 8 *Includes only fluids without … Continue reading Paediatric Anaesthesia Formulas – 1
When hypothermic cardiopulmonary bypass (HCPB) or deep hypothermic circulatory arrest (DHCA) is used during cardiac surgery, anesthesiologists and perfusionists are faced with an important question: Should one temperature correct blood gasses to patient temperature (pH-stat) or not (α-stat)?
What happens in Hypothermia?
The solubility of CO2 and O2 in blood is affected by temperature. At lower temperatures, solubility is increased, leading to a reduction in partial pressure. Blood gas analyzers measure gas partial pressures at 37° C. As blood from a hypothermic patient is warmed to 37° C by the analyzer, CO2 and O2 come out of solution, leading to Paco2 and PaO2 higher than those present in the patient.
Think of a shaken soda bottle. The liquid is under greater pressure when it has been agitated to bring the CO2 out of solution. Leave it alone in the refrigerator and it will be like nothing ever happened. The CO2 didn’t go anywhere, but the PCO2 decreased by cooling the bottle and letting the CO2 go back into solution.
Blood gas analyzers make use of algorithms to correct the reported values to the patient’s actual temperature.
The hemoglobin’s affinity for oxygen increases as temperature decreases (hemoglobin-dissociation curve is shifted left). Solubility of O2 is also increased in hypothermia. But the calculated oxygen content of blood varies very little in temperature variation. The American Association for Respiratory Care recommended against the routine correction of blood gas samples for temperature.

Two strategies have been developed for the management of arterial gas partial pressures during management of hypothermic patients such as during hypothermic cardiopulmonary bypass (HCPB) or deep hypothermic circulatory arrest (DHCA): alpha-stat and pH-stat.
Alpha-Stat Hypothesis
In aqueous systems, neutrality (pN) is said to occur when [H+] = [OH−]. The dissociation of water H2O=[H+]+ [OH–] depends on temperature; therefore, the pH value at which pN occurs varies with the temperature.
The mean intracellular pH of man is 6.8 at 370C which is indeed the pH of neutrality (pN) at that temperature!
So pN is temperature dependent and if the hypothesis (ICF pH = pN) is correct then intracellular pH should change with change in temperature to maintain the predicted relationship.
But intracellular pH is maintained at about pN with change in temperature!! HOW?
It is thought that protein buffering is largely responsible for maintaining this temperature pH relationship. Specifically, the imidazole group of the amino acid histidine has a dissociation constant (pKa) value similar to that of blood. Therefore, if carbon dioxide stores are held constant during cooling, the ionization state (termed alpha) will remain constant.
Adjustment of ECF pCO2 is necessary as this maintains a constant relative alkalinity of the ECF (pH 7.4) relative to the ICF (pH 6.8) so there is constancy of the gradient for H+ across the cell membrane. In reality this does not mean that ventilation has to increase markedly with decrease in temperature because the reduced metabolic rate will automatically result in decreased CO2 production.
Alpha-stat strategy maintain intracellular electrochemical neutrality across all temperatures. This may be important because the ionization state affects both the structure and the function of proteins.
The ‘Alpha’ is the ratio of protonated to total imidazole of histidine residues among the protein molecules. It is expressed as a ratio or percentage. It At 37°C, at the normal intracellular pH of 6.8, alpha is approximately 0.55; that is to say approximately half of the imidazole and histidine residues are protonated. T.J. Morgan from Oh’s Manual reports to us that this 0.55 alpha value is optimal for intracellular enzyme structure and function, and that maintaining this optimal value should be a goal of therapy.
Alpha-Stat (temp uncorrected):
When a patient is cooled during hypothermic cardiac bypass, and measurements are made at the patient’s actual temperature, pH will increase and the measured pCO2 and the pO2 will decrease with lowering of the patient’s temperature.
When blood drawn from a patient undergoing CPB at 18° C is measured in a blood gas machine, which anaerobically warms the sample to 37° C and reports values at normothermia.
With alpha-stat management, one would strive for normal temperature-uncorrected results i.e. paCO2 and the pH are maintained at 40 mmHg and 7.40 when measured at 37 C (i.e. blood sample is warmed to normothermia for measurement)
Lower PaCO2 is targeted than for the pH-stat approach. The alpha-stat approach targeting lower PaCO2:
Disadvantages of alphastat include less efficient and less homogeneous cooling and less reduction of oxygen consumption.

pH-stat (temp corrected):
An alternative strategy is the pH-stat approach to acid-base management. The pH-stat strategy endeavors to maintain a constant pH despite changes in temperature. During bypass, decreasing blood temperature increases the solubility of carbon dioxide and, consequently, results in decreased Paco2 values. Therefore, the perfusionist must either decrease the “sweep speed” of the air-oxygen mixture or, less commonly, add carbon dioxide to the oxygenator ventilation system to increase the carbon dioxide content and maintain a Paco2 of 40 mm Hg (and normal pH) as the temperature of the blood decreases.
PaCO2 is maintained at 40 mmHg and the pH is maintained at 7.40 when measured at the patient’s actual temperature (hypothermia)
Carbon dioxide is a potent cerebral vasodilator; therefore, the increase in carbon dioxide content during pHstat management
Which Strategy Is Best?
Studies have compared the two strategies with respect to outcomes, with varying results. In general, clinical studies support the use of pH-stat management in pediatric cardiac surgical procedures during HCPB or DHCA. In adult patients, the use of alpha-stat management is supported for HCPB. For procedures involving DHCA in adults, use of pH-stat management has been suggested to increase the rate and uniformity of cooling and alpha-stat management during rewarming.
Ref:
Miller’s Anesthesia, Eighth edition.
Effects of pH Management During Deep Hypothermic Bypass on Cerebral Microcirculation: Alpha-Stat Versus pH-Stat. Circulation September 24, 2002
TemperatureCorrectionof Blood-Gasand pH Measurements. CLIN.CHEM.29/11, 1877-1885(1983)
Alpha-stat and PH-stat Models of Blood Gas Interpretation. http://www.derangedphysiology.com
Kerry Brandis’ Chapter 1.6 – Alpha-Stat Hypothesis
Arterial Blood Gas in Hypothermia. LITFL

1.It is important to ensure that hypertension is well controlled, seizure prophylaxis is initiated, and volume status is optimized. Fluid management in the patient with preeclampsia is complicated by the … Continue reading Pre-eclampsia – Ten Rules for Anaesthesia Consideration
Physiologic fundamentals
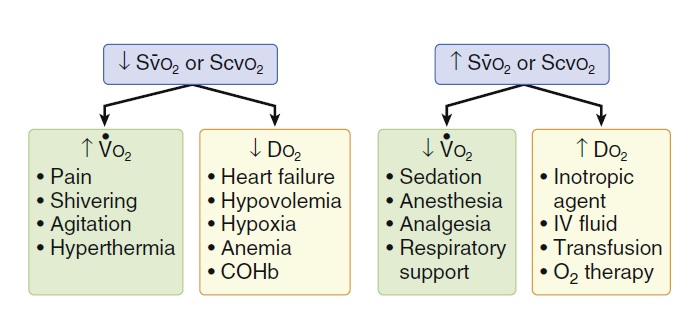
Mixed venous oxygen saturation (SvO2) is the percentage of oxygen bound to hemoglobin in blood returning to the right side of the heart. This reflects the amount of oxygen “left over” after the tissues remove what they need. It is used to help us to recognize when a patient’s body is extracting more oxygen than normally. An increase in extraction is the bodies way to meet tissue oxygen needs when the amount of oxygen reaching the tissues is less than needed.
A true mixed venous sample (called SvO2) is drawn from the tip of the pulmonary artery catheter, because pulmonary artery catheter use has declined dramatically, ScvO2 measurements obtained from internal jugular or subclavian catheters are often used and interpreted in the same manner. An ScvO2 refers to a central venous sample. An ScvO2 measurement is a surrogate for the SvO2. It may be used to identify changes in a patient’s tissue oxygen extraction.
Normal SvO2 60-80%. Normal ScvO2 (from an internal jugular or subclavian vein) is > 70%.
Mixed venous saturation SvO2 is a measure of the balance between global oxygen delivery and uptake.
If the amount of oxygen being received by the tissues falls below the amount of oxygen required (because of an increased need, or decreased supply), the body attempts to compensate as follows:
The cardiac output is increased in an effort to increase the amount of oxygen being delivered to the tissues. Oxygen Delivery is the amount of oxygen being sent to the tissues, and is determined by the following:
Oxygen Delivery (DO2) = Cardiac Output (HR X Stroke Volume) X Oxygen Content (Hb X SaO2)
If this is not sufficient to meet tissue energy needs, second compensation come in to play
Tissues begin to remove or extract a higher percentage of oxygen from the arterial blood. This results in a reduced amount of oxygen remaining in the blood as it returns to the right side of the heart (decreased SvO2). If this is not sufficient to meet tissue energy needs, third compensation come in to play.
If the tissues fail to receive an adequate supply of oxygen, anaerobic metabolism becomes the only mechanism to produce tissue ATP. Anaerobic metabolism is inefficient, producing a large amount of metabolic waste (e.g. lactic acid) that is difficult for the body to eliminate quickly. It also produces a relatively poor supply of ATP. Prolonged anaerobic metabolism leads to energy depletion and metabolic acidosis.
VO2 (Oxygen Consumption) = Cardiac Output X Hb X (SaO2 – SvO2)
There are 4 fundamental causes for a drop in SvO2:
Measurement Principles:
The measurement of venous O2 saturation can be performed intermittently by co-oximetry of blood sampled from the distal tip of a pulmonary artery catheter (SvO2) or a central venous catheter (Scvo2). Venous saturation can also be measured continuously by spectrophotometry. Specialized venous oximetry catheters are available for both pulmonary artery and central venous monitoring and have the advantage of providing continuous measurements of O2 saturation.
Applications and Interpretation:
In patients undergoing major abdominal as well as cardiac surgical procedures, intraoperative reductions in SvO2 and Scvo2 have been associated with postoperative complications.
Scvo2-guided, protocol-based, goal-directed therapy is advocated for the management of sepsis.
Mixed venous saturation SvO2 is a measure of the balance between global oxygen delivery and uptake.
Ref:
Miller’s Anesthesia, Eighth edition.
Stephen J. Shepherd, Rupert M. Pearse; Role of Central and Mixed Venous Oxygen Saturation Measurement in Perioperative Care. Anesthesiology 2009;111(3):649-656.
Brenda Morgan. Clinical Educator, CCTC. London Health Sciences Centre.

Typically, surgical repair of the cleft lip is performed at 3 to 6 months and the repair of the cleft palate at 9 to18 months of age. Pharyngoplasty, performed for … Continue reading Cleft Lip / Palate – Ten Rules for Anaesthesia Consideration

Preoperative interventions in patients with COPD aimed at correcting hypoxemia, relieving bronchospasm, mobilizing and reducing secretions, and treating infections may decrease the incidence of postoperative pulmonary complications. Smoking should be … Continue reading Chronic Obstructive Pulmonary Disease – COPD – Ten Rules for Anaesthesia Consideration

Goal: Preload is normal or increased. Afterload is normal. Goal is controlled ventricular response. Avoid tachycardia, pulmonary vasoconstriction The most important hemodynamic goal is to avoid tachycardia (keep heart rate … Continue reading MITRAL STENOSIS – Ten Rules for Anesthesia Considerations

Goal: Maintain preload and diastolic filling. Maintain sinus rhythm. Maintain or increase afterload. Avoid myocardial depression. Avoid tachycardia, hypotension, and increased myocardial oxygen demand situations. In the absence of CHF, … Continue reading AORTIC STENOSIS – Ten Rules for Anesthesia Considerations

Brochard (2002) defines intrinsic PEEP as “unintentional or un-measured end-expiratory hyperinflation”. Definition: Expiration usually occurs as a passive movement Resistance to air flow (eg. bronchospasm) results in decreased expiratory flow … Continue reading Auto PEEP